Updated Resource: Commercial Payers’ Use of Oncology Compendia
Summary
Our updated dashboard provides insights into trends in commercial payers’ use of clinical drug compendia for off-label oncology coverage decisions.Payers use clinical drug compendia such as the National Comprehensive Cancer Network Drugs & Biologics (NCCN) Compendium and Elsevier’s Clinical Pharmacology to classify drugs and biologics (“drugs”) in formularies and to guide medical appropriateness of use.
The compendia for Medicare and Medicaid are dictated in federal law, while the compendia for commercial payers vary by state and their own coverage rules. Until now, commercial payers’ use of clinical drug compendia has not been available in one place, making it difficult to assess the impact on patient access.
Introducing an Updated Dashboard of Compendia
Payer-specific interpretations of compendia create coverage disparities, leading to treatment delays. To address this challenge, Avalere Health has developed an updated Payers’ Overarching Compendia Policies Dashboard to help stakeholders anticipate restrictions and understand evolving policies.
This new dashboard reflects sizeable shifts in the commercial payer market driven by industry consolidation and realignment. It tracks off-label oncology trends across 32 of the top 50 payers, covering 209 million lives—a 65% increase from the 127 million covered lives in last year’s report.
As plans continue to consolidate and shift, the composition of the top 50 plans will evolve. Being able to target specific plans year over year will enable manufacturers to maintain focus on the most influential payers and adapt engagement strategies to shifting market dynamics.
Because clinical drug compendia are essential—but inconsistently applied—this resource empowers users to advocate for fair, evidence-based access and minimize treatment delays. It also serves as a practical tool for reimbursement hotlines and account managers to address coverage denials or fill policy gaps when payer criteria are unclear.
Dashboard Components
The dashboard identifies which compendia are referenced by payers, alignment with other compendia or sources recognized by the Centers for Medicare and Medicaid Services, and evidence ratings that influence coverage.
Users can filter by compendium rating (e.g., NCCN Category 2B) to assess coverage variations for drugs and support market access strategies, payer engagement, and denial analysis. Users can also filter for payer-specific evidence ratings which may support evidence generation/submission strategy for denied claim appeals.
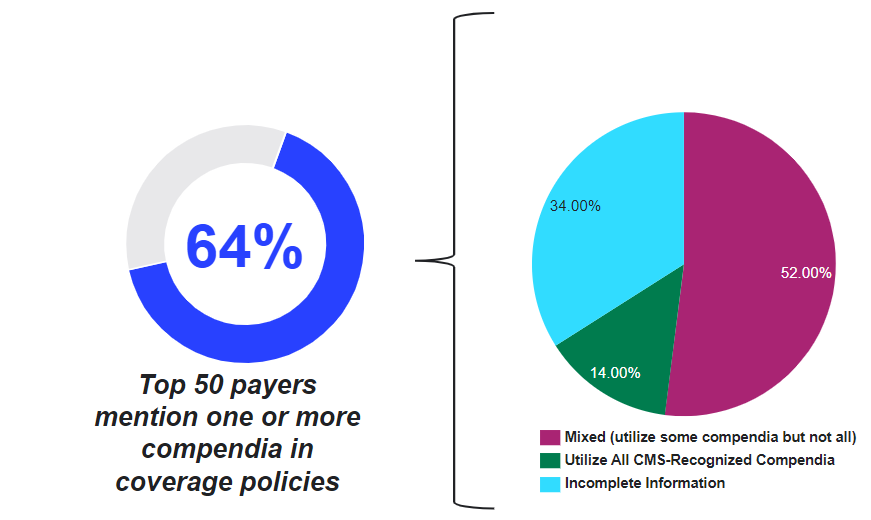
Figure 1. Commercial Payers’ Use of CMS-Recognized Compendia
Access The Report
Avalere Health’s experts in compendia, commercialization, regulatory, and policy strategy can help manufacturers, patient advocacy organizations, payers, and other stakeholders analyze the clinical coverage policies and access implications to off-label treatments and help develop strategies to mitigate delays in patient access to treatment.
To purchase the report or speak with an Avalere Health expert, contact Amy Schroeder at amy.schroeder@avalerehealth.com.




