Revisiting Medicaid Work Requirements
Summary
Federal policymakers are considering Medicaid work requirements as a mechanism to reduce spending; recent state experiences offer important considerations.Background
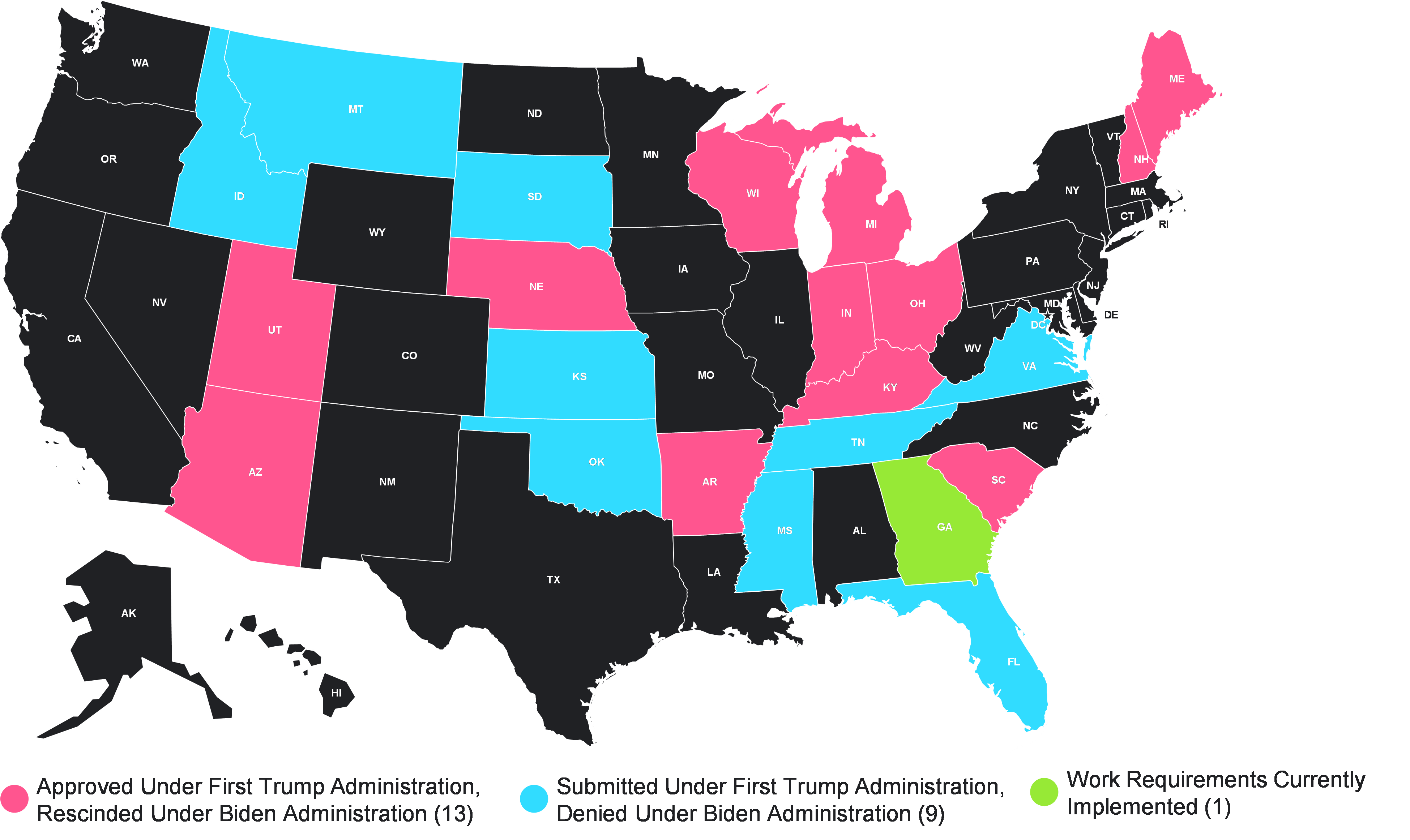
Work requirements condition Medicaid eligibility on the completion and reporting of a minimum number of hours (typically 20–80 hours/month) spent working or in other approved activities. During President Trump’s first term, 13 states received federal approval to establish work requirements within their Medicaid programs (see Figure 1). Of those states, just two (AR and GA) undertook implementation. Arkansas’s requirements were subsequently halted by a federal court in 2019, after less than a year in effect. Georgia’s implementation was allowed to proceed by a different court’s ruling, and its work requirements remain in effect.
Figure 1. Historical and Current Status of Work Requirement Waiver Requests
As Congress looks to advance a budget reconciliation vehicle this year focused on tax cuts, defense, and border security, it will need to identify significant cost offsets. The Medicaid program is likely to be a potential target for savings, with a variety of Medicaid policies under consideration, ranging from changes to the federal matching rate, reforms to program financing like a per capita cap, or changes to eligibility through work requirements. Establishing work requirements in Medicaid, potentially on a mandatory basis across states, has the potential to gain momentum. Accordingly, as policymakers and stakeholders assess these options it is important to understand state experiences that may inform the policy design and broader debate.
Population Subject to Requirements: The criteria for defining what populations will be subject to work requirements influence how impactful the policies may be. Some past waivers focused work requirements on non-disabled, non-pregnant, working-age adults earning up to 100% of the federal poverty level (FPL), while others applied to the entire Medicaid expansion population (earning up to 138% of FPL). While most approved waivers were in states that had already expanded Medicaid following the ACA, GA included work requirements in its Medicaid partial expansion proposal. All approved waivers exempted specific sub-populations, with variation in populations across states.
Exceptions and Work Alternatives: Previous state approaches have allowed individuals to request an exception to work requirements, which can provide some flexibility and mitigate against unintended eligibility loss. CMS guidance in 2018 required states to exempt medically frail individuals and individuals with acute medical conditions from work requirements and to consider other factors (i.e., high unemployment, caregiving responsibilities) in designing work requirements. States also frequently recognize other activities, like volunteering, education, or job training, in lieu of work.
Implementation and Reporting: States adopted varied approaches for individuals to demonstrate compliance with requirements, which have direct implications for program enrollment. Some states required monthly reports while others proposed to verify compliance annually. Some allowed reports by phone or in person, in addition to an online portal. Arkansas, for example, phase -in its program by age group (first ages 30–49 then 19–29). Indiana gradually increased its hourly requirements from zero to 20 hours per week over 18 months.
Consequences for Non-Compliance: Individuals who do not comply with work requirements would lose Medicaid eligibility under most proposals. Some states allowed a grace period before initiating disenrollment. States may have included lockouts as well, which prevent disenrolled individuals from reenrolling within a certain period.
Outcomes and Implications
Medicaid enrollment was impacted in both states that implemented work requirements. Over 18,000 individuals were disenrolled in less than a year in AR, while GA’s Medicaid expansion had enrolled roughly 6,900 adults through the end of February 2025 out of the hundreds of thousands estimated to potentially be eligible. The Congressional Budget Office (CBO) projected that a federal work requirement would decrease Medicaid enrollment, estimating that the Limit, Save, Grow Act of 2023 (H.R. 2811) would result in 1.5 million adults losing Medicaid coverage.
Current policy discussions are focused on the federal savings associated with work requirements that can help support other priorities through a budget reconciliation package. The CBO estimates savings of more than $100 billion under a nationwide (federal) work requirement. Experience in AR and GA highlights potential fiscal impacts for states (i.e., new implementation and oversight costs). Losses of Medicaid enrollment may have implications for other state and federal government programs, along with stakeholders throughout