Opportunities to Move the Needle on US Behavioral Healthcare in 2025
Summary
Behavioral health is at a turning point in 2025, with newly implemented policies, groundbreaking treatments, and novel regulatory and financial dynamics.Background
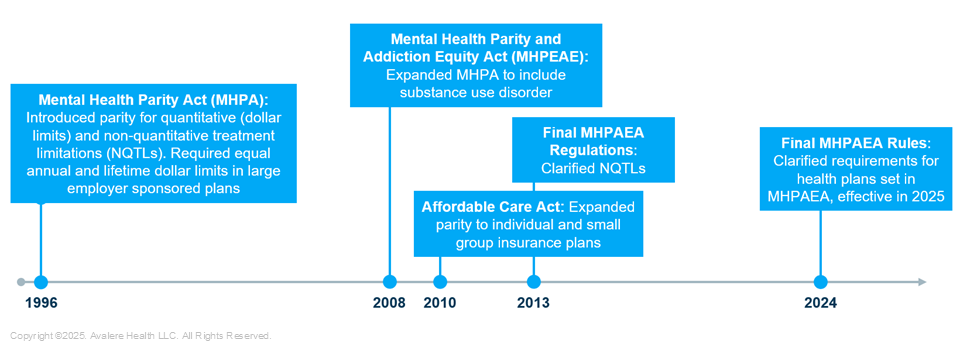
Despite policy efforts over the last three decades to enhance access to and quality of US behavioral healthcare (see Figure 1), patients still face unmet needs and suboptimal outcomes. There is a continuum of services addressing behavioral health conditions and substance use disorders (SUDs), but access remains fragmented and is complicated by barriers such as narrow provider networks, provider shortages, limited reimbursement for services and products, and high patient out-of-pocket costs for specific treatments.
Figure 1: Mental Health Parity and Addiction Equity Act (MHPAEA) Timeline
Behavioral health stakeholders are at a critical turning point in 2025: policies finalized in 2024 are now being implemented, groundbreaking treatments are emerging, and key stakeholders are navigating growing regulatory and financial pressures. Yet, with these challenges come significant opportunities to drive improvements in access, equity, and innovation.
2024 Parity Rule
A major shift comes with the Mental Health Parity and Addiction Equity Act , which was passed in 2008 but not been enforced. In 2024, the Biden administration finalized a new rule imposing stricter requirements to ensure that behavioral health benefits truly match medical benefits. While patient advocacy groups applauded the rule, employer groups and payers are grappling with potential compliance challenges and the risk of litigation over enforcement ambiguities. For stakeholders, stronger parity enforcement may lead to expanded coverage in the therapeutic area, potentially increasing access.
Psychedelic Treatment Landscape
Meanwhile, the landscape for ketamine treatment and the broader psychedelic category is evolving rapidly with the Food and Drug Administration’s (FDA) recent approval of Spravato for monotherapy use in patients with treatment-resistant depression. Regulatory uncertainties remain, however. The FDA has granted breakthrough therapy designations to psilocybin-assisted therapy for major depressive disorder (MDD) and post-traumatic stress disorder (PTSD), yet its recent rejection of a MDMA-based PTSD therapy over safety and data concerns signals a cautious stance. The agency’s decision raises the bar for future approvals, emphasizing the challenge of balancing innovation with patient safety.
Meanwhile, Colorado’s 2025 rollout of a new psilocybin regulatory framework could set a precedent for state or even federal policy. The development of next-generation psychiatric treatments poses risks and opportunities for stakeholders, emphasizing the importance of clinical engagement and policy advocacy.
Investment in Behavioral Health
Over the past five years, there has been increased demand for virtual care, policy shifts expanding mental health coverage, and heightened investor interest in behavioral health, all coalescing in a surge of behavioral health investments in 2025.
In its Calendar Year 2025 Medicare Physician Fee Schedule Final Rule, CMS finalized three new HCPCS codes providing Medicare payment for supply, onboarding, and use of “digital mental health treatment devices.” Venture capital flowed into digital behavioral health startups during the pandemic, but many companies continue to face reimbursement challenges and sustainability concerns.
The competitive landscape for branded MDD drugs is also becoming more intense, and manufacturers are positioning new therapies in response to shifting payer policies. At the same time, employer demand for behavioral health solutions continues to grow.
New Administration and Congress
The new Trump administration will play a role in reshaping behavioral health policy priorities. While the Biden administration focused on behavioral health parity enforcement and expanding Medicaid funding, the new administration could bring different approaches. On February 13, President Trump issued an executive order Establishing the President’s Make America Healthy Again Commission that aims to address the rising burden of chronic and mental health conditions, which drive 90% of US healthcare costs. The initiative seeks to investigate root causes, improve public health, and reduce economic and national security risks linked to poor health outcomes.
Additionally, Congressional dynamics will be pivotal while bipartisan efforts to expand behavioral health coverage continue. Funding debates and broader healthcare policy shifts could stall progress. Changes in federal policy could impact drug pricing negotiations, Medicaid funding for treatment, and the long-term commercial viability of novel therapies.
Future Opportunities
Despite ongoing uncertainties, 2025 marks a significant period for behavioral healthcare policy and innovation. Payers and policymakers are focused on implementing new coverage pathways for emerging treatments, while providers aim to reduce emergency department visits for behavioral health crises and address disparities in access and affordability. Industry stakeholders emphasize the importance of maintaining telehealth flexibilities and expanding digital solutions to support continuity of care. As a result, many in the healthcare ecosystem anticipate that the coming year will bring notable developments that could shape long-term behavioral health policy and infrastructure.
Avalere supports stakeholders across the behavioral healthcare spectrum, and can partner with stakeholders as they:
- Shape mental/behavioral health policy initiatives
- Identify systemic pain points and identify collaborative solutions
- Engage in or create opportunities for shared dialogue across stakeholders
- Advocate for broader access to innovative, life-saving treatments
For further information and to connect with industry experts, connect with us.




