Digital Health Evolution in Remote Monitoring and AI Codes
Summary
Evolving digital health codes are reshaping how technology and care connect.Digital healthcare is rapidly transforming how care is delivered and paid for. Remote patient monitoring (RPM) improves patient engagement, access, and outcomes; reduces hospital visits and cost; and supports care in chronic disease, post-surgery, and diverse settings. Remote therapeutic monitoring (RTM) evolved out of RPM to better capture and reimburse the remote monitoring of therapy-related patient parameters beyond just physiological data.
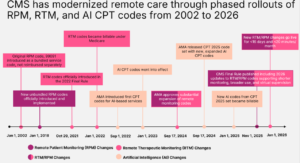
In recent years, coding for PRM and RTM has expanded. The digital health space has gone from one with no applicable codes, to codes without reimbursement, and now to the development of more sophisticated structures that recognize RPM, RTM, and AI-supported care.
While reimbursement remains inconsistent across payers and programs, meaningful progress has been made. Understanding and adapting to these ongoing changes is vital for providers, payers, and digital health innovators aiming to align technology-driven care models with reimbursement frameworks that sustain innovation, encourage adoption, and support long-term value.
Expansion of RPM and RTM Codes
RPM coding has evolved over the last two decades. In 2002, there was physician-only billing with CPT code 99091, which allowed limited reimbursement for reviewing remote physiological data. In 2018, the American Medical Association (AMA) introduced a comprehensive coding framework with codes 99453, 99454, and 99457 for device setup, data transmission, and management. Coding expanded further during the COVID-19 pandemic in 2020 with code 99458 to cover additional clinical management time by broader care teamsCOVID-19 further accelerated adoption and policy flexibility surrounding RPM, normalizing remote monitoring across diverse care settings. In 2024, the Office of Inspector General identified significant oversight and compliance gaps in Medicare’s RPM program, prompting calls for stronger safeguards. In 2026, CMS will release updates aiming to enhance program stability and broaden clinical applicability across both RTM and RPM as digital and AI-assisted care grows.
The AMA introduced RTM codes in 2021 to address gaps in monitoring therapy effectiveness, patient adherence, and functional outcomes, areas not fully covered by RPM codes. These codes capture data relevant to musculoskeletal therapy, respiratory therapy, behavioral health, and medication adherence. Now with six distinct codes (CPT codes 98975–98981), RTM allows rehabilitation professionals and other providers to bill for remote engagement, reflecting evolving care delivery models emphasizing patient functional status and therapeutic progress.
Starting January 1, 2026, the Centers for Medicare and Medicaid Services (CMS) will allow billing for RTM and RPM with reduced minimum patient data collection days (2–15 days instead of 16) and shorter management times (as little as 10 minutes), expanding use to shorter care episodes and broadening eligible providers to include a wider range of clinicians involved in multidisciplinary remote care. These changes expand RPM and RTM use to shorter care episodes such as post-surgical recovery and episodic conditions.
Integration of AI-Augmented Codes into Digital Medicine
The 2026 CPT updates mark the first comprehensive incorporation of AI-augmented medical codes, although the codes were first discussed in 2022. The seven new codes cover specialties including radiology, pathology, cardiology, and diagnostics, recognizing the transformative role of AI in assisting with clinical decision making, image and pattern analysis, predictive analytics, and workflow automation. This update marks a foundational milestone for AI in medicine, enabling proper documentation, billing, and adoption of AI-enhanced healthcare services starting January 1, 2026. As AI applications expand, continued refinement of coding to capture new AI capabilities and associated work will be critical to supporting adoption and investment in digital health technologies.
Figure 1. CMS has Modernized Remote Care Through Phased Rollouts of RPM, RTM, and AI CPT Codes
Navigating Regulatory and Reimbursement Landscape
CMS and private payers continue to expand RPM and RTM coding frameworks but apply varying payment, coverage, and billing rules. For manufacturers, this underscores the need to align technology use cases and service models with payer expectations. Demonstrating clinical value and cost-effectiveness through real-world data is becoming essential for market access, as coverage policies increasingly hinge on measurable outcomes and appropriate coding alignment. In our next Insight, we will explore the coverage shifts and examine how payer policies for RPM are evolving.
Partner With Us
Avalere Health combines deep coding, clinical, and market expertise to turn reimbursement strategies into improved patient access. We closely monitor regulatory and coding developments to help life sciences companies optimize coverage for digital health, remote monitoring, and AI-enabled services. Partnering with Avalere Health ensures insight-driven strategies that enhance access and outcomes. To learn more about how we can assist you, connect with us.
CPT ©2025 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.




