
Federal and State Policy
As the largest US healthcare payer, the federal government plays a dominant role in shaping the healthcare marketplace, while states take center stage when it comes to developing novel policy approaches. Our experts track, interpret, and model policies that affect insurance coverage, access, and consumer choice so you can see around the bend.


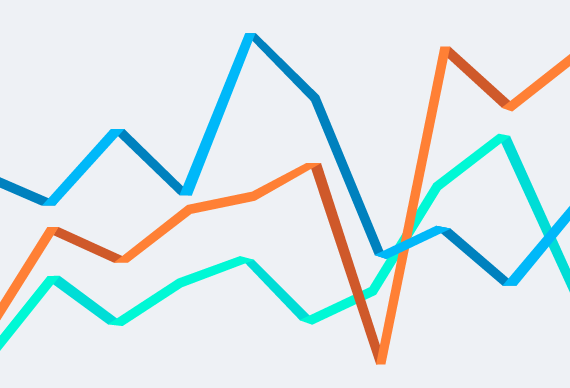
Only 33 Percent of Exchange Enrollees in 2016 Kept Their Same Plan from 2015
One third of those who enrolled in a health insurance plan on Healthcare.gov this year picked the same plan as last year, according to a new analysis from Avalere. In total, 3.2 million of the 9.6 million exchange shoppers in 2016 kept their previous plan.
Proposed Changes to Part D Would Increase Beneficiary Costs
Avalere Experts Estimate MedPAC Proposal to Change Calculation of Part D Enrollees' True Out-of-Pocket Spending Would Increase Beneficiary Costs by $4.1 Billion Between 2017-2020

Changing the Way Insurers are Paid Could Increase Stability in the Exchange Market and Beyond
New Avalere report identifies opportunities to refine the risk-adjustment model that could improve the way Affordable Care Act plans are paid
Right-to-Try Bills Grow in Popularity yet Success Is Unclear
Almost every state has introduced Right-to-Try bills to try to offer patients another avenue to access investigational drugs outside of the Food and Drug Administration's (FDA) expanded access program. However, it is unclear whether these laws will impact patient access given their questionable legal standing, reduced patient protections due to lack of FDA oversight, and the risks to manufacturers of providing products under Right-to-Try laws.

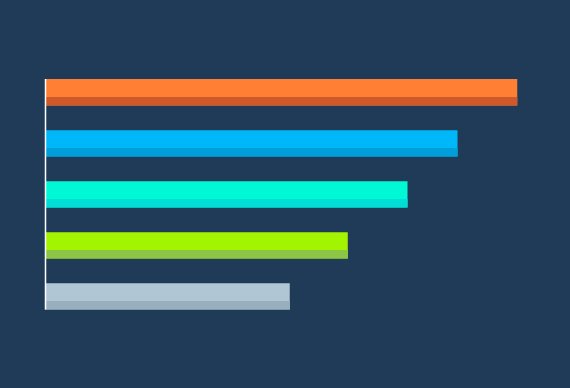
More than 70 Percent of Medicare Advantage Enrollees in Plans with Four or More Stars
Percentage of Medicare Advantage enrollees in plans with at least four stars continues to grow.
Majority of Drugs Now Subject to Coinsurance in Medicare Part D Plans
Percentage of drugs in Part D plans that require coinsurance increased significantly since 2014. Medicare Advantage plans require coinsurance far less often than Part D plans.
Veterans Administration and California Medicaid Drug Lists Cover Less than 60 Percent of Drugs Available to California Public Employees
The CalPERS Basic Plan Drug List, which is the formulary for all California public employees, includes 222 brand drugs and 287 generic drugs. In contrast, drug coverage in the Veterans Administration (VA) and Medi-Cal (California's Medicaid program) is far more limited than the CalPERS drug list.

Avalere’s Take: President Obama’s FY2017 Healthcare Budget
President Obama released his budget for the 2017 fiscal year today. Avalere offers the following observations on the healthcare proposals:
Exchange Enrollment Is on Track to Meet Administration’s Goal
Today, the Department of Health and Human Services (HHS) announced that 9.6 million individuals selected a health insurance plan on HealthCare.gov during the recent open enrollment season. Avalere estimates that 2016 year-end enrollment will slightly exceed the Obama administration's goal of enrolling 10 million people.
Spotlight On: Patient Access to Oncology Care in Exchange Plans
In an article published in The American Journal of Managed Care, Avalere's Caroline Pearson and Deirdre Parsons examine provider networks and benefit design for oncology care in health insurance exchanges.
Prescription-Only Pseudoephedrine-Containing Products Contribute to Growing Primary Care Physician Shortage
According to a new analysis by Avalere, a prescription requirement for pseudoephedrine-containing products also fuels the growing shortage of primary care physicians, thereby increasing the cost, time, and difficultly of obtaining the treatment for legitimate users.

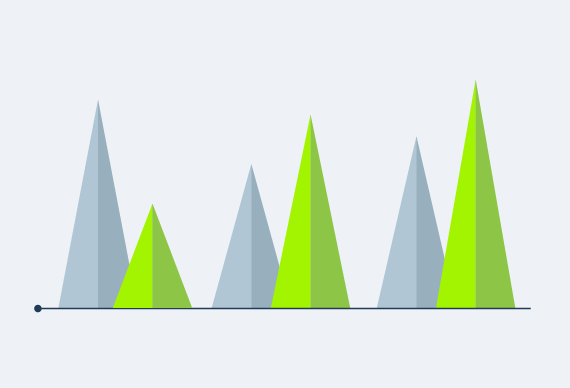
Nearly 60 Percent of New Medicare Advantage Plans Are Sponsored by Healthcare Providers
A new analysis from Avalere Health finds that hospitals and health systems are increasingly taking risk for the cost of Medicare patients and the quality of the care they receive.
Federal Government Underpays Medicare Advantage Plans for Enrollees with Multiple Diseases
A new analysis by Avalere finds that the Centers for Medicare and Medicaid Services (CMS) underpay Medicare Advantage (MA) plans for the costs of treating individuals with multiple chronic conditions.
Proposed Exchange Standardized Benefit Designs Expand First-Dollar Coverage for Services and Drugs
As the government considers rules for 2017 insurance plans offered through exchanges, a new analysis by Avalere finds that proposed 2017 benefit designs could increase coverage of certain services and drugs, while lowering out-of-pocket costs for many consumers.
MACRA and the Promise of Better Patient/Family Engagement in Post-SGR World
The story of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) actually begins in the previous millennium. In 1997, when the Congress passed the Balanced Budget Act, it ushered in the era of the Sustainable Growth Rate (SGR) formula. In theory, the SGR payment adjustment would raise or lower physician reimbursement each year based on spending relative to the target SGR. The caveat, however, was that Congress had the authority to suspend or adjust this benchmark, a "patch" that they regularly deployed through a "doc fix" for nearly two decades.
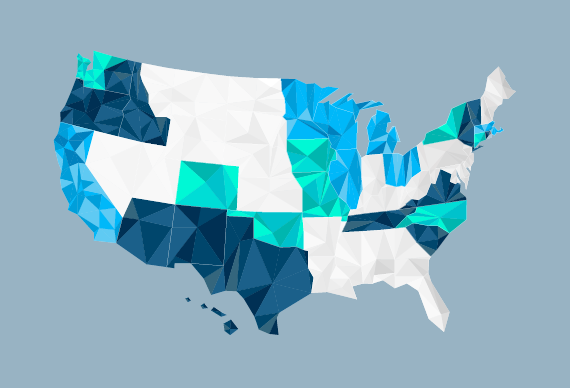
Where Are the States Going on Payment and Delivery Reform? Tracking SIM Grant Developments
Believing that states are productive incubators of innovation, the Center for Medicare & Medicaid Innovation (CMMI) launched a State Innovation Model (SIM) grant program in 2013 to encourage state-by-state testing of innovative payment and delivery models.
Business Education for Healthcare Innovation
The healthcare delivery system is one of the most complex businesses in the country.
Medicare Drug Plans Favor Generic Opioids that Lack Abuse Deterrent Properties
New research from Avalere finds that despite the innovation of abuse-deterrent properties and labeling for branded opioids, Medicare Part D plan coverage for these products is declining rapidly.
An Analysis of the Impact of Breakthrough Therapies on Government Spending
To evaluate public program spending on new medications in the drug development pipeline, Avalere projected the fiscal impact of 10 FDA breakthrough therapies to Medicare, Medicaid, and the health insurance exchanges created by the Affordable Care Act (ACA).

Upcoming Managed Care Regulation Will Impact Plans Serving 46M Medicaid Beneficiaries
Over the past four years, enrollment in Medicaid managed care has increased by 48 percent, with 46 million beneficiaries now receiving coverage through these plans. The government will soon update regulations that direct the plans providing this coverage.





