Sociodemographic Factors and Healthcare Costs Among Rare Epilepsies
Summary
Distinct patient characteristics and cost profiles across rare epilepsies reinforce the value of disease-specific approaches in rare disease research.Background and Study Context
Rare diseases are often perceived as clinically and economically homogeneous due to small patient populations and overlapping features. However, this perception can overlook critical differences in how different rare disease patients interact with the healthcare system. A new analysis of three rare epilepsies among Medicare fee-for-service (FFS) beneficiaries illustrates how even clinically similar conditions diverge in sociodemographic patterns and cost outcomes.
Using the 100% sample of Medicare FFS claims from 2018–2022 linked to ZIP code–level socioeconomic data from Acxiom’s Market Indices, Avalere Health identified patients with Lennox-Gastaut Syndrome (LGS), Dravet Syndrome (DS), and Tuberous Sclerosis Complex (TSC) to examine patterns in demographic characteristics, social determinants of health (SDOH), and per patient per month (PPPM) healthcare costs across the three conditions. Although formal statistical testing was not completed, thematic differences in descriptive results are described below.
Key Findings
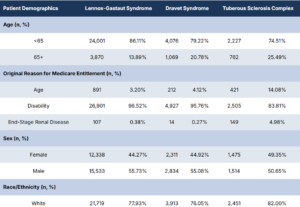
Patient Demographics Factors Vary by Condition: Medicare FFS beneficiaries with LGS, DS, and TSC differ in meaningful ways across demographic factors (see Table 1 below), including:
- Age: LGS and DS populations skew younger than TSC, with more patients aged less than 65 (86.11% and 79.22% compared with 74.51%) and nearly all patients qualifying for Medicare through disability (96.52% and 95.76%, respectively, compared with 83.81%). In contrast, TSC includes a broader age range, with a larger proportion of beneficiaries qualifying based on age compared with LGS and DS (14.08% compared with 3.20% and 4.12%, respectively).
- Sex: While men represent a slight majority across all groups, a higher proportion of patients with TSC are female than in LGS and DS (49.35% compared with 44.27% and 44.92%, respectively).
- Race: A higher proportion of beneficiaries with DS are Non-White compared with patients with LGS and TSC. Specifically, 16.29% of included patients with DS are Black, compared with 13.45% and 10.10% among patients with LGS and TSC, respectively.
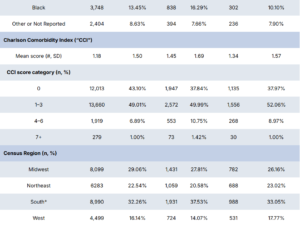
- Comorbidities: DS patients appear to experience the highest number of comorbidities, as measured through the Charlson Comorbidity Index (CCI). Even when comparing the similarly aged LGS and DS groups, patients with DS have an average CCI score more than 22% higher than that of LGS patients (1.45 vs 1.18). Further, a higher proportion of patients with DS have a CCI score of 4–6 compared with patients with LGS and TSC (10.75% compared with 6.89% and 8.97%, respectively).
- Location: A higher proportion of patients with DS live in the South compared to patients with the other conditions, while patients with LGS are more frequently living in the Midwest than those with DS or TSC. These regional differences may reflect disease prevalence, but could also indicate variations in diagnosis, referral patterns, or access to specialists.
Table 1. Patient Demographics Among Medicare FFS Beneficiaries with Rare Epilepsies
*Includes patients with unknown census region (<11)
Socioeconomic Differences Across Conditions:There are also differences in individual and near-neighborhood level SDOH factors among Medicare FFS beneficiaries with LGS, DS, and TSC, including:
- Medicaid and Low-Income Part D Subsidy Eligibility: Patients with LGS and DS are more likely to have full or partial dual-eligibility for Medicare and Medicaid than patients with TSC (95.71% and 95.39%, respectively, compared with 80.29%). Relatedly, patients with LGS and DS are also more likely to have full eligibility for a Low-Income Part D Subsidy, compared to those with TSC (96.41% and 96.03%, respectively, compared with 82.77%).
- Household Income and Neighborhood Federal Poverty Level (FPL): On average, patients with DS have a lower median household income than those with LGS or TSC ($56,424 compared with $59,072 and $59,583). Similarly, a higher proportion of the neighborhoods of patients with DS are below the FPL.
- Health Professional Shortage Areas (HPSAs): More patients with DS live in a neighborhood designated as a full Health Professional Shortage Area compared with patients with LGS and TSC, although it is common across rare epilepsy patients. Over 92% of LGS, DS, or TSC patients live in a neighborhood with an HPSA designation.
- Rurality: A higher portion of patients with LGS live in an urban neighborhood compared to patients with DS and TSC who are more concentrated in rural and suburban neighborhoods.
Healthcare Costs and Cost Drivers Differ by Condition: PPPM costs post-diagnosis also differed by condition, both in magnitude and drivers of costs. Total PPPM healthcare spending was highest for TSC compared with LGS and TSC (see Table 2 below). Additionally, the proportion of PPPM costs driven by medical vs. pharmacy spend also differed by condition. Patients with DS had a higher proportion of spend due to medical spending (67%) vs. pharmacy spending, followed by LGS (59% medical) and TSC (47% medical).
| Condition | Total PPPM Spend | Medical PPPM Spend (% of total) | Pharmacy PPPM Spend (% of total) |
|---|---|---|---|
| TSC | $3,582 | $1,695 (47%) | $1,886 (53%) |
| LGS | $3,389 | $1,990 (59%) | $1,399 (41%) |
| DS | $3,291 | $2,196 (67%) | $1,096 (33%) |
*Represented RxHCCs also have the largest percentage changes in relative risk score factors in the Community, LIS ≥ 65 Mode
Implications for Stakeholders and Conclusion
Although rare diseases such as LGS, DS, and TSC, may share clinical features, they diverge in who they affect, where patients live, and how those patients utilize care. Specific demographic and SDOH characteristics may reveal potential barriers to early diagnosis and ongoing access or could indicate certain disease risk factors. These findings serve as a case study for rare epilepsies and the rare disease landscape as a whole and demonstrate the importance of disease-specific research.
For stakeholders such as manufacturers, payers, providers, and policymakers, these findings reinforce the importance of:
- Evaluating the condition-specific burden of disease
- Designing tailored evidence generation strategies<//li>
- Aligning access and reimbursement models with disease-specific needs
- Incorporating SDOH and real-world data into program and policy decisions
Grouping rare epilepsies or other rare diseases together may simplify the narrative but doing so can mask unique differences in each patient group. These results underscore the importance of condition-specific research to understand the nuances between diseases that may otherwise be evaluated collectively to support targeted HEOR strategies, tailored value propositions, and informed payer engagement.
Dive Deeper
At Avalere Health, we apply our expertise in evidence generation and commercialization strategies to help stakeholders ensure patient access to treatments for rare diseases. To learn more about how Avalere can help you understand the unique dynamics impacting rare disease assets and conduct research in this patient population,connect with us.
Funding for this research was provided by Jazz Pharmaceuticals. In particular, Junji Lin and Michael Faithe contributed to the design and execution of the study. Avalere Health retained full editorial control.
This analysis utilized the 100% Medicare FFS claims, accessed by Avalere Health via a research collaboration with Inovalon, Inc. and governed by a research-focused CMS Data Use Agreement.