2027 Advance Notice Materially Alters Part D Risk Adjustment
Summary
Proposed updates to the Part D risk adjustment model to further separate MA-PDs and PDPs will change plan payments for certain conditions if finalized.On January 26, the Centers for Medicare & Medicaid Services (CMS) released the Calendar Year (CY) 2027 Medicare Advantage (MA) and Part D Advance Notice. The Advance Notice is an annual regulatory document that describes the agency’s proposed payment and coverage policies for MA and Part D plans for the upcoming plan year.
In addition to MA plan payment and Part D benefit parameter updates, this year’s Advance Notice includes major changes to the Part D risk adjustment model. Specifically, CMS proposes to create separate Prescription Drug Hierarchical Condition Category (RxHCC) model segments for Medicare Advantage Prescription Drug plans (MA-PDs) and standalone Prescription Drug Plans (PDPs). CMS notes that this update is intended to improve the model’s predictive accuracy for both MA-PDs and PDPs.
Overview of Part D Risk Adjustment
CMS uses the RxHCC model to predict plan liability for prescription drugs. Specifically, the model predicts drug costs based on the health status, medical diagnoses, and demographic characteristics of a plan’s enrollees (e.g., age, sex, low-income status, institutionalized status). Currently, the RxHCC model includes separate model segments based on factors including residence (i.e., community vs. long term institutional care), low-income status, reason for eligibility (e.g., age vs. disabled status), and whether the beneficiary is newly enrolled in Medicare.
Changes to the RxHCC model can affect how accurately CMS payments align with actual plan costs for specific beneficiary types and for enrollees with particular health conditions. It is therefore critical for stakeholders to understand how the proposed changes to the CY 2027 model will affect the accuracy of payments, plan economics, plan benefit and formulary strategies, and other behavior changes impacting Part D beneficiaries, drug manufactures, and health plans.
Proposed Updates to the CY 2027 Part D Risk Adjustment Model
Beginning with CY 2025, CMS implemented separate normalization factors in Part D risk adjustment for PDPs and MA-PDs. In addition to continuing the separate normalization factors, the agency’s proposed update to the CY 2027 RxHCC model would also create separate model segments for beneficiaries enrolled in MA-PDs vs. those enrolled in PDPs. This would be a change from previous years, where each model segment was applied to all beneficiaries regardless of the plan they were enrolled in. If finalized, this update to the RxHCC model would change plan prescription drug payments for particular diagnosis groups based on the type of plan a beneficiary enrolls in.
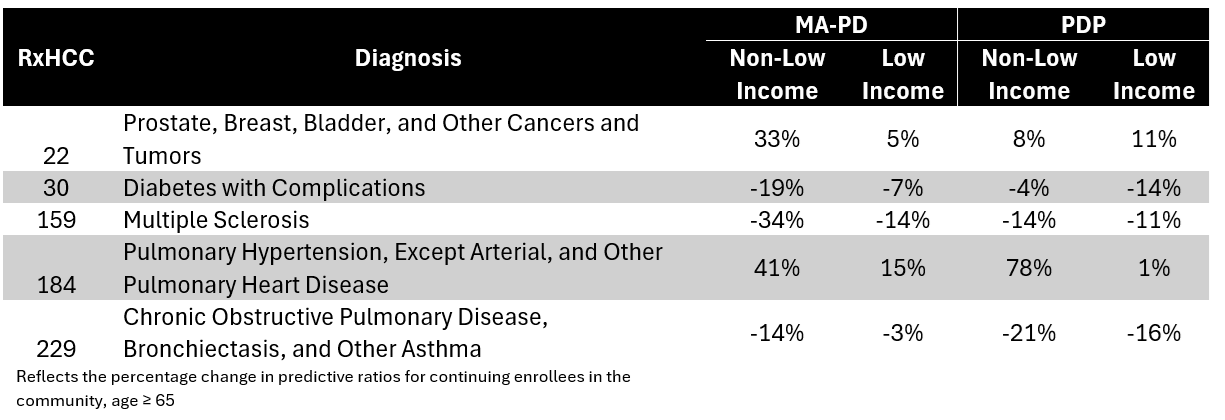
Avalere Health conducted preliminary analysis to compare the predictive ratios under the proposed 2027 updates to the RxHCC model and the current RxHCC model. Table 1 provides the percentage change in predictive ratios for common diagnoses between CY 2026 and the proposed update for CY 2027. Changes in the predictive ratios for a specific diagnosis will directly result in plan payment changes for that diagnosis.
Table 1. Percentage change in predictive ratios for select conditions under 2027 Advance Notice proposal compared to current RxHCC model
As the portion of plan payments financed through risk-adjusted payments has increased under Part D benefit design, stakeholders should consider key implications of the proposed model changes, including:
- The extent to which the updates will affect the delicate balance between actual plan costs and payment amounts for MA-PDs vs. PDPs, especially for the diagnoses most impacted.
- How changes in plan payments vs. actual costs may impact plan formulary and benefit strategies.
- Whether the proposed changes could meaningfully change the trajectory of the PDP market, which has eroded over the past several years.
Methodology
Avalere Health identified the predictive ratios for each RxHCC diagnosis group from the RxHCC Model Relative Factors for Continuing Enrollees tables published in the 2026 Rate Announcement and the 2027 Advance Notice. Avalere Health also identified the MA-PD and PDP Normalization Factors in the 2026 Rate Announcement and 2027 Advance Notice. The percentage change was calculated after adjusting each predictive ratio by the normalization factor for the corresponding plan type and contract year.




