Early Enrollment Data Indicates More Beneficiaries Could Benefit from MPPP
Summary
Avalere Health’s analysis of early MPPP enrollment shows that only a small portion of beneficiaries who are likely to benefit from the program have enrolled.The Medicare Prescription Payment Plan (MPPP), a program launched in January 2025 under the Inflation Reduction Act (IRA), offers a new option to help beneficiaries with high out-of-pocket (OOP) costs manage their drug spending over the plan year. However, the recent implementation of the MPPP and lack of beneficiary awareness of the program may be contributing to lower enrollment in the early months of 2025.
Guidance from the Centers for Medicare & Medicaid Services (CMS) on MPPP implementation sets guidelines for plan outreach and education to beneficiaries. In addition to including MPPP information in standard plan materials, plans must conduct targeted outreach to enrollees who incurred $2,000 or more in OOP costs in the first three quarters of 2024. Plans were required to send the CMS-developed “Likely to Benefit” notice to the beneficiaries who met this threshold by December 7, 2024. This notice provides information on the MPPP and informs beneficiaries that they may benefit from enrolling in the program. However, enrollment in the MPPP is not automatic, and beneficiaries must take action to opt in through their plan.
Beneficiaries Identified as Likely to Benefit from the MPPP
Avalere Health’s analysis of Part D claims data finds that over 1.2 million beneficiaries met the $2,000 OOP spending threshold in the first three quarters of 2024 and should have received the MPPP “Likely to Benefit” notice. Of the 1.2 million beneficiaries meeting this threshold, approximately 440,000 (35%) were enrolled in Medicare Advantage Prescription Drug Plans (MA-PDs) and over 800,000 (65%) were in standalone Prescription Drug Plans (PDPs).
Early Enrollment in the MPPP and Opportunities for Stakeholders
Early data for 2025 indicates that a small portion (15%) of the beneficiaries who were flagged as likely to benefit from the MPPP have enrolled in the program. As of the end of February 2025, Part D Drug Event (PDE) data shows that only about 190,000 beneficiaries who filled a script in January or February 2025 were enrolled in the MPPP, including about 70,000 PDP and 120,000 MA-PD beneficiaries (Figure 1).
While MA-PD enrollees accounted for just over one-third (35%) of enrollees identified as likely to benefit from the MPPP based on 2024 OOP spending, they represent two-thirds of MPPP enrollees in early 2025. Of the PDP and MA-PD enrollees who were identified as likely to benefit based on 2024 OOP spending and who filled a script in January or February 2025, only 9% of PDP beneficiaries are enrolled in the MPPP compared to 27% of MA-PD beneficiaries (Figure 1).
Figure 1. Number of PDP and MA-PD Beneficiaries Enrolled in MPPP vs. Identified as Likely to Benefit and Not Enrolled
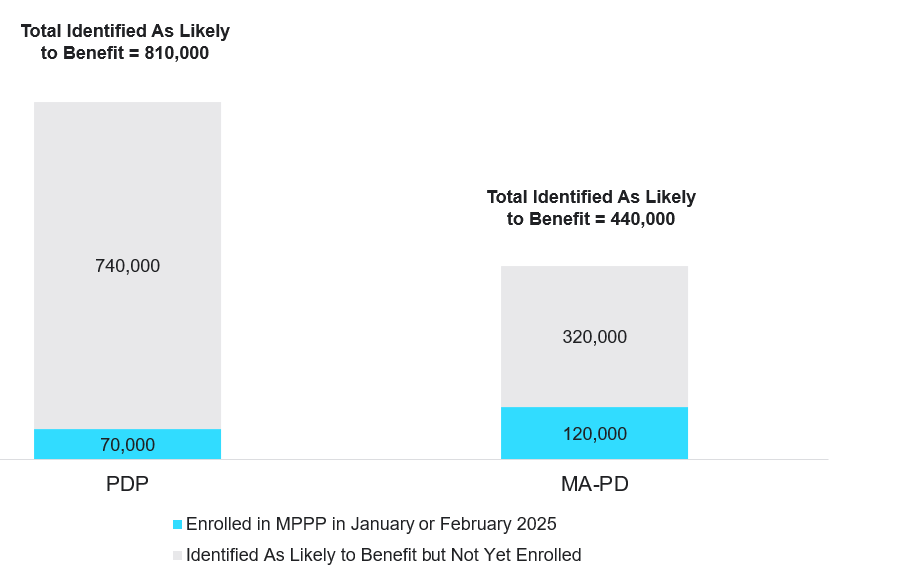
Note: Enrollment in the MPPP in 2025 reflects only beneficiaries who had a PDE claim in January or February.
A previous Avalere Health analysis found that among beneficiaries projected to reach the 2025 OOP cap, about 9% of enrollees would do so in January or February with about half of beneficiaries reaching the cap before September. This indicates that more beneficiaries could benefit from the MPPP as they continue to fill scripts in the coming months. However, beneficiaries with certain conditions are more likely to reach the cap earlier in the year and may benefit from early enrollment in the MPPP. For example, a separate Avalere Health analysis found that among beneficiaries with a rare form of cancer who were projected to reach the OOP cap in 2025, more than 40% were projected to reach the cap within the first three months of the year.
While these initial MPPP enrollment data only provide initial indicators of uptake in the program, they highlight strategic opportunities for stakeholders. For manufacturers, education for beneficiaries and other stakeholders, along with other changes to support tools and eligibility criteria as part of manufacturer patient assistance programs, can help drive sustained uptake of the MPPP. Other stakeholders, such as patient groups, plans, and pharmacies should consider strategies to support enrollment in the MPPP.
Avalere Health’s experts are working closely with stakeholders to understand the complexities of the MPPP and Part D redesign, as well as develop strategies to support patient access and affordability in this market. To learn more connect with us.
Methodology
This analysis utilized Medicare data through an agreement with CMS, wherein Avalere Health has access to CMS’s Chronic Condition Warehouse Virtual Research Data Center (“VRDC Data”). The analysis includes all Part D beneficiaries, including low-income subsidy (LIS), non-LIS, and Employer Group Waiver Plan enrollees, with a script filled in 2024 or in January or February of 2025. Beneficiaries were identified as enrolled in the MPPP if they had a script in the Part D PDE where MPPP enrollment was indicated. Avalere also analyzed beneficiaries who were either diagnosed with COVID-19 or filled a prescription for a COVID-19 medication, finding that over 110,000 beneficiaries met the $2,000 OOP spending threshold in the first three quarters of 2024. Of these, 10% of beneficiaries had enrolled in the MPPP as observed in the January and February 2025 Part D PDE data. Analysis of enrollees with rare form of cancer reaching the OOP cap is based on 2021 PDE data.




